- Pediatric Darp Notes Examples
- What Is A Darp Note
- Darp Notes Examples
- Nursing Darp Notes
- Writing Darp Notes
When Notes are required: Notes are to be written in SOAP format. S=Subjective data. O=Objective data. A=Assessment. P=Intervention/Plan SOAP is to be used by all Interprofessional team members including nurses. Narrative ( chronological) Notes:.When no appropriate powerform can be found for the situation. Jun 23, 2014 For example, I will want a larger space to take notes on the interventions that I have done, as compared to documenting the goal of the session. After choosing a font, I modify the text so it is large and transparent (I tell InDesign to make it 40% transparent so I can write over these prompts).
Creating effective notes for your therapy sessions doesn’t have to be a daunting task. Many clinicians have found that using DAP notes is the best way to take notes in a quick, useful, and effective manner. Of course, before using DAP notes you’ll need to understand the basics behind them and get a few tips for how you can use the technique for your notes.
DAP Notes Basics

The first step in writing DAP notes is understanding the format. Let’s evaluate each section.
D – Data
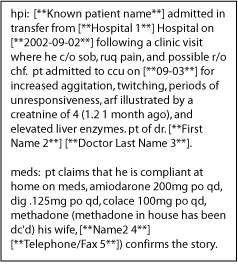
When used in medical settings, the “DAP” in DAP notes stands for “Diagnostic Assessment Program.” When you use DAP note examples in healthcare institutions, you would follow the standard format that includes data, assessment, response, and a plan for the medical care of your patients. Jan 16, 2020 DARP means Data Action/nursing decision, Response, Plan. Additionally, what is charting by exception? Charting by exception (CBE) is a shorthand method of documenting normal findings, based on clearly defined normals, standards of practice, and predetermined criteria for assessments and interventions. Below is a fictional example of a progress note in the SOAP (Subjective, Objective, Assessment, Plan) format. For the purposes of this sample progress note, the focus is on the content of the progress note, rather than the format. The sample offers examples of what the SAPC QI and UM.
When writing in this section you’ll want to take note of what you observed during the session. This could be any relevant behavior, especially those that might affect the way you proceed with treatment.
A – Assessment
After you’ve recorded the relevant behaviors, you’ll use this section to understand what those behaviors mean. Essentially, you’ve collected your data and now you need to analyze it. What do you think that action or actions mean?
P – Plan
Pediatric Darp Notes Examples
This is the final piece of your note-taking puzzle. You’ve gathered data through observation, you’ve assessed the data accordingly, and now you’ll use what you’ve learned to record the treatment plan for your patient.
That’s the basics of DAP notes. It's simple enough, right? Of course, you want to use the technique in a way that’s beneficial to you.
3 Tips for Making DAP Notes Work
1. Define Your Perfect Note
When writing your notes, it helps to understand what perfection looks like to you. Yes, your notes will not be perfect, because no note truly is, but you need to understand the outcome you’re looking for before you can know if you got close to it. We’ve already defined each section and what guidelines say they should have, once you decide to use this method you have to tailor that information to fit your needs. Ask yourself – What information do I need about my patient and this session to be able to create a plan for them? If someone else were writing these notes, what information would I find usable and helpful?
After you’ve answered these questions for yourself you can begin to determine how each section of your therapy notes should look. For instance, maybe your data section contains phrases that are only 3 to 5 words in length to give you quick details of what you see while your assessment section features longer sentences that provide the detail you need regarding what you wrote in the data section. What matters is that each section allows you to use the information contained there in a quick and effective manner.
2. Keep It Simple
What Is A Darp Note
You want to get as much valuable information from your notes as possible, but you don’t want to overcomplicate them. Start getting familiar with the information you don’t want to include in your notes and the information you need to include. You don’t need to record that you adjusted the temperature as your patient entered the room, but you may want to note your patient’s demeanor as they greeted you. What you want to avoid is a bunch of words on the page that look thorough but ultimately can’t be used. This may take some practice, but it’s a habit you’ll be happy you developed.
3. Use the Tools that Work Best for You
Another piece of the process you need to consider is what you’ll be using to take your notes. Is it more effective for you to use an online template to take notes or would you prefer writing your notes on paper then transferring them online? When you’re deciding which is best for you, you’ll want to keep the result you’re working towards in mind. Are your handwritten notes sloppy and hard to understand? Do you find that you can’t type as fast as you think? You might have to work with both for a while before you get a handle on the best method to use going forward.
If you aren’t sure which method works best for you, you can always start with templates that you can either print or use online. Using a template will give you the opportunity to make sure you are recording the information you need each time. If you use the same template on and off-line, you’ll have the opportunity to gauge which technique works best for you (and saves you the most time). You can also take things a step further and use a HIPAA compliant EHR that allows you to record and save notes for future review.
If you’re interested in the ways that My Client’s Plus can help you with note-taking or other aspects of your practice, don’t hesitate to sign up for a free trial or contact us for more information.
This is the third post in a series that highlights standardized formats for your clinical notes. The series began here.
Darp Notes Examples
A second format for documenting your clinical work is called DA(R)P notes, sometimes referred to as DAP notes. These are similar to clinical SOAP notes.
DA(R)P is a mnemonic that stands for Data, Assessment (and Response), and Plan.
Data, in this format, includes both subective and objective data about the client as well as the therapist’s observations and all content and process notes from the session.
Nursing Darp Notes
The Assessment and Response includes your clinical impressions, hunches, hypotheses, and rationale for your professional judgment. Progress is also noted here.

Writing Darp Notes
Plan refers to your original treatment plan and any response / revisions needed based on your most recent interactions with your client.
This method of clinical note taking is also an acceptable format for your documentation.
Tomorrow I’ll talk to you about BASIC SID notes.